The Lebanese Healthcare Crisis

Our Mission
Overview of the Healthcare Crisis in Lebanon
Timeline of Major Events
Economic Crisis Worsens
Widespread government corruption and overspending combined with a stagnating economy led to spiraling inflation, default on debts, and a liquidity crisis. The resulting halt in foreign investment further amplified these issues and led to a rapid collapse of the national currency and GDP.
Beirut Port Explosion
After confiscated explosives sat in the port for 6 years, a small nearby fire detonated one of the biggest non-nuclear explosions in history, resulting in 218 deaths, over 7,000 injuries, and more than 300,000 newly homeless people from an avoidable tragedy.
Continuing Impacts
The resulting and rapidly escalating economic crisis has grown to deeply affect every sector of the economy, especially the salaries of workers and operations of businesses. The brain drain of professionals has severely weakened the healthcare system and reduced the quality of care.
Through a Statistical Lens
The Brain Drain
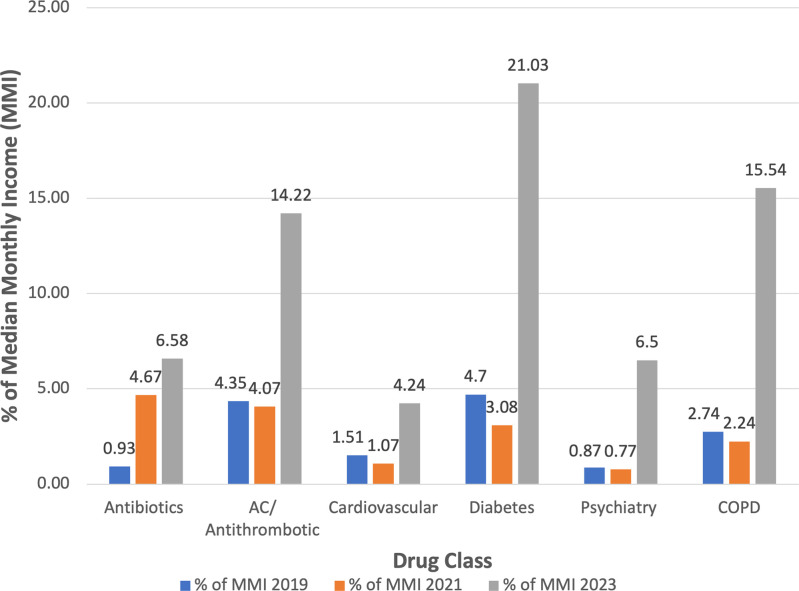
Medication Costs
Personal Stories

Dr. Aya Farès
Hematologist & Oncologist
Aya works at Rizk hospital in Beirut and is an outspoken advocate for the medical crisis.

Mohammed Qassem
Lebanese Citizen & Father

Solutions for The Future
The Brain Drain
Medication Costs
Foundational Longer-Term Solutions
Advocacy Initiatives
Lessons for Our Healthcare System
Specific Strategies Include:
Longer Duration Prescriptions
Access to Specialists
Primary Care Referrals
Detailed Breakdown of Medication Coverage
Prescribing Generics
Addressing Anxiety and Concerns
Get Involved!
Specific Organizations Include:
Doctors Without Borders
Lebanese Red Cross
International Medical Corps
AmeriCares Global Emergency Response
MedGlobal
Project Lifeline
About the Author